Advance Care Planning

National Advance Care Planning Week.
From 18 to 24 March 2024, we encourage you, regardless of your age or health, to make your health care preferences known. Or, for some, start to think about what your preferences may be.
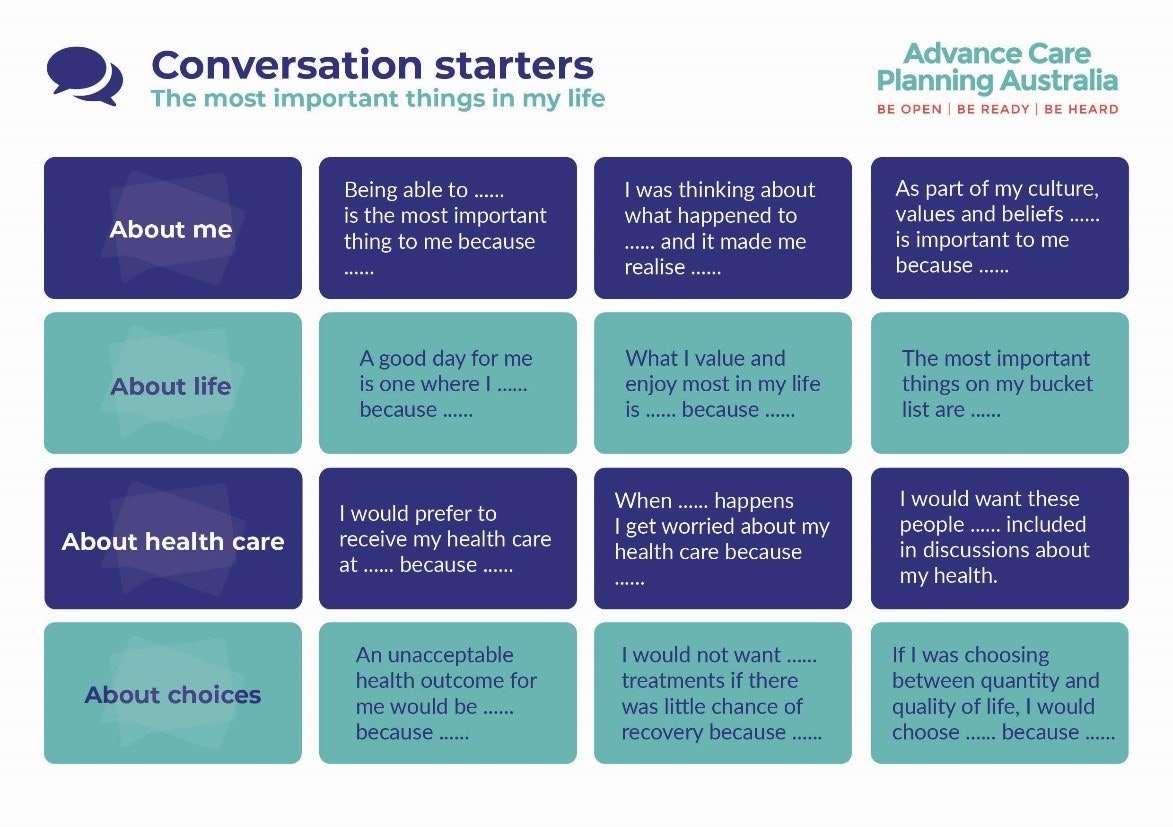
Discuss with your loved ones about not only your preferences, but theirs as well. Open a conversation. Some simple Conversation starters:
This year’s Advance Care Planning Australia’s campaign ‘challenges everyone to discuss what living well means to you and to consider who you would want to speak for you, if you could no longer communicate or make your own health care decisions.’ (*Advancedcareplanning.org.au)
Why it's important
Advance care planning benefits everyone: you, your family, carers and health professionals.
- It helps to ensure you receive the care you actually want
- It improves ongoing and end-of-life care, along with personal and family satisfaction
- Families of people who have undertaken advance care planning have less anxiety, depression, stress and are more satisfied with care
- For healthcare professionals and organisations, it reduces unnecessary transfers to acute care and unwanted treatment
If you haven't documented your preferences or identified a substitute decision-maker, and you become seriously ill or injured, doctors will make treatment decisions based on their assessment of your best interests. This may include treatments that you would not want.
Planning is for everyone
Everyone should consider advance care planning, regardless of your age or health. Ideally, you should start planning when you're healthy - before there's actually an urgent need for a plan.
It's a team effort
Advance care planning requires a team effort. It involves having conversations with your family, friends, doctors, care workers and other health professionals. Having these conversations will help you start thinking about what's important to you.
The process
Advance care planning doesn't need to be complicated but it does require careful consideration. It involves thinking about your values and preferences for care and acceptable outcomes, talking about them with others, appointing someone to make decisions on your behalf and documenting everything.
Important links
HNE Health Pathways: https://hne.communityhealthpathways.org/
CC Health Pathways: https://centralcoast.communityhealthpathways.org/
Patient Info HNE: HNE Patientinfo.org.au
Patient Info CC: Central Coast Patientinfo.org.au (ccpatientinfo.org.au)
Advance Care Planning Australia: Advance Care Planning Australia
This section contains information, links and resources about advance care planning for patients, carers, GPs and health professionals. Information about palliative care can be found here.
Health professionals have a key role in talking with patients about their values, future health goals and treatment preferences while they are still relatively well and able to participate.
Responsibilities of health professionals
As part of Advance Care Planning (ACP), general practitioners and nursing staff are responsible for:
- Identifying existing documents and/or Medical Treatment Decision Maker (MTDM) and accurately recording details,
- Providing patients with information about ACP,
- Discussing health issues, condition, treatment options, prognosis and ACP,
- Encouraging discussion with the patients’ MTDM and involving the MTDM/family (where possible and appropriate),
- Helping a patient document their Advance Care Directives (ACD) (if required), checking draft documents, and helping clarify wording or intentions,
- Recording discussions about ACP in medical software and ensuring others can access this information if needed,
- Storing copies of ACP-related documents, including ACD in medical records so they are accessible when needed,
- Sharing information about the patient’s ACD with others involved in their care (with patient consent) - such as hospital or specialists,
- Encouraging patients to give copies of their ACD to anyone who may be involved in making decisions about their care and to upload copies of the ACD to their My Health Record,
- Ensuring information is available if care is needed after hours (for example, by a medical deputising service/locum service),
- Regularly reviewing ACD particularly if a patient’s situation changes, and
- Activating (enacting) the ACD when needed including using ACDs to inform medical treatment and care decisions if the patient loses capacity.
Health professionals should note that:
- There is no dedicated Medicare Benefits Schedule (MBS) item for Advance Care Planning (ACP). Several MBS items can support ACP as part of other health interventions (e.g., a 75+ health assessment or chronic disease management plan).
- Advance Care Planning Australia (ACPA) provides information and resources to healthcare professionals, individuals, and care workers, and an advisory service (M-F during business hours - 1300 208 582). It has also developed a guide for the use of Medicare Benefits Schedule items for ACP. For eligibility criteria and service requirements refer to MBS Online.
- RACGP’s position statement clarifies how advance care planning should be incorporated into routine general practice.
Links to information and resources
This section contains links to information and resources about advance care planning for GPs and health professionals.